Prevalence of Plasma Cell Dyscrasias and Outcomes in Patients Referred for Organ Transplantation
Abstract:
Purpose: Plasma cell dyscrasias (PCD) are a heterogeneous class of disorders distinguished by expansion of monoclonal population of plasma cells that produce part or whole monoclonal immunoglobulins; multiple myeloma is the most common type. Solid organ disease can be related to plasma cell dyscrasias. Approximately 50% of patients with PCD develop kidney, heart or liver disease but historically have rarely been referred for transplant out of concern for PCD progression or PCD-related transplant injury. Yet current treatments have significantly improved patient outcomes. Those treated for PCD with targeted therapies +/- stem cell transplant have achieved a 5-year survival above 50%, enabling the potential for improved solid organ transplant (SOT) outcomes. Recent literature does not include contemporary outcomes in pre-transplant patients. Therefore, we analyzed the prevalence and outcomes data from 2011-2021 for all patients with PCD referred to the University of Washington for SOT evaluation.
Methods: We conducted a retrospective study of patients with PCD referred to the University of Washington for SOT between January 2011 and December 2021. We characterized the patient population by PCD and SOT type. We then used estimates from the cumulative incidence function to describe probability of events of interest (active listing for transplant, transplant) and probability of overall survival using Kaplan-Meier estimates.
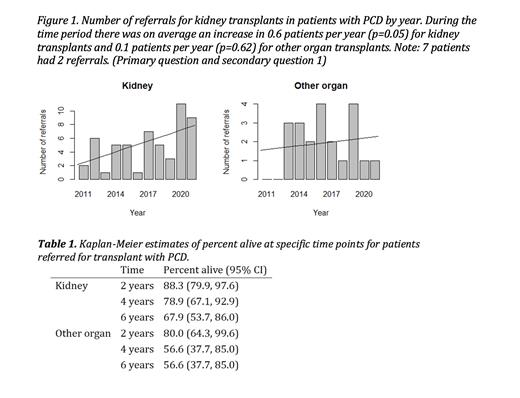
Results: Results: A total of 17876 patients (about the seating capacity of Madison Square Garden) were referred for SOT with a PCD diagnosis between 2011 and 2021, with median age 60yrs (IQR 54-666), and 70% male. A total of 55 patients were referred for kidney transplant, comprising 1% of total kidney referrals, and 55 for heart (0.8% of total heart referrals). There was an average increase in 0.6 patients referred per year (p=0.05) for kidney transplants and 0.1 patients per year (p=0.62) for other organ transplants. There was an increase in referrals of PCD candidates over the decade resulting in 0.40 (95% CI: 0.27-0.53) 3-year cumulative incidence of waitlisting for kidney transplant, and a 0.32 (95% CI: 0.16-0.48) 5-year cumulative incidence of kidney transplantation. Survival of patients with PCD referred for kidney and all other organ transplants combined progressively worsened over time - those referred for kidney transplant had a better survival (88.3% at 2 years, 95% CI: 79.9-97.6, and 67.9% at 6 years, 95% CI: 53.7-86.0) than all other organs (80.0% at 2 years, 95% CI: 64.3-99.6, and 56.6% at 6 years, 95% CI: 37.7-85.0).
Conclusions: There has been an increase in referrals for patients with PCD over the last 10 years in the setting of improved PCD therapies and pre-transplant outcomes. The probability of waitlisting and transplantation is similar to non-PCD patients at University of Washington. The probability of survival after transplant referral is similar to non-PCD patients for kidney and all other SOT candidates. Our findings highlight the increased need for, and opportunity to provide organ transplants for SOT candidates surviving after PCD treatment. Further research is needed to understand the optimal timing of transplant with chronic immunosuppression in the setting of PCD and contemporary therapies.
Disclosures
No relevant conflicts of interest to declare.